Dental trauma
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Aim
To guide Emergency Department (ED) staff in the assessment treatment and appropriate referral of patients with dental trauma.
Priorities1,2
- Orofacial injuries are, by definition, head injuries. Assess for neurological signs of a head injury.
- Oral wounds are dirty wounds. Check tetanus immunisation status.
- Management of avulsed permanent teeth is time critical. See the section on avulsion. Call the Dental team from Triage.
- Although dental injuries can have profound, life-long consequences for the patient, they are rarely life threatening, so will be triaged as non-urgent. To improve timely access to care, please contact the on-call dentist early to discuss management, rather than leaving the patient waiting. They will usually be managed by the Dental team rather than the medical team.
- The on-call Paediatric Dentist will deal with teeth and supporting structures.
- The on-call Oral and Maxillofacial Surgeon will deal with all facial bone fractures including the temporomandibular joints and the orbits.
Assessment
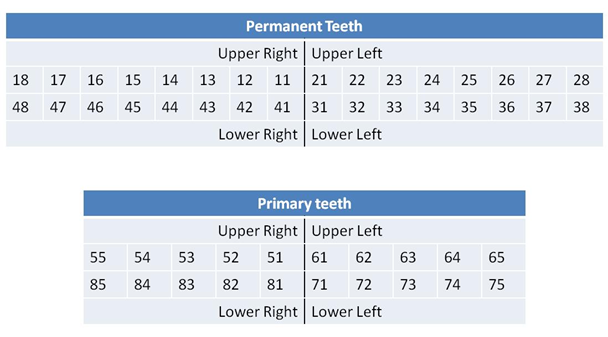
Use the following numbering system to describe the affected tooth or teeth.
- Consider non accidental injury (NAI) in children with unexplained oral injuries including dental trauma, particularly in non-mobile infants
- All injury presentations in children under 2 years must have an Early Childhood Injury Proforma (MR301.3) completed (internal WA Health only)
Haemorrhage
- The child who has had recent extractions may suffer from a secondary haemorrhage from the extraction site.
Management
- Ensure adequate pain control has been administered.
- Wash out the patient’s mouth with cold water and remove blood clots with a gauze swab to identify the source of bleeding.
- Position the patient so their head is elevated and place a gauze swab in the mouth so direct pressure is applied to the bleeding site and ask the patient to bite firmly and steadily for 20 minutes.
- They should not ‘chew’ the gauze.
- If bleeding is not controlled in 40 minutes (2 gauze swabs), the dentist should be contacted.
Fracture of the facial bones including the orbits
Management
The dentist on call should be notified immediately after the diagnosis is made, even if the other injuries are the main problem. The dentist will assess the patient and consult with the duty Oral and Maxillofacial Surgeon.
Dental and supporting tissue injuries
|
|
 |
|
|
|
 |
- Contact PCH Dental team for their opinion
|
- Commence fasting
- Refer to PCH Dental team for opinion
|
 |
- Refer to PCH Dental team for opinion
- Keep any tooth fragment in sodium chloride 0.9%
|
- Commence fasting
- Refer to PCH Dental team for opinion
|
 |
- Contact PCH Dental team for their opinion
|
- Refer to External Dental Service.
- Supply chlorhexidine 0.5% oral gel BD for 1 week.
|
 |
- Refer to External Dental Service.
- Supply chlorhexidine 0.5% oral gel BD for 1 week.
|
- Commence fasting
- Refer to PCH Dental team for opinion
|
 |
- Refer to PCH Dental team for opinion
- Analgesia
- Gently reposition
- Stabilise
|
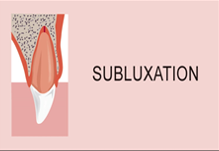
- Mild mobility, no occlusal interference: Refer to External Dental service.
- Otherwise, fast and refer to PCH Dental team for opinion.
- Supply chlorhexidine 0.5% oral gel BD for 1 week.
|
 |
- Refer to PCH Dental team for opinion.
- Supply chlorhexidine 0.5% oral gel BD for 1 week.
|
- If > 50% commence fasting
- Refer to PCH Dental team urgently
|
 |
If > 50% contact PCH Dental team urgently
|
- Confirm tooth found / investigate.
- Do not replant.
- Refer to External Dental services.
- Supply chlorhexidine 0.5% oral gel BD for 1 week.
|
 |
- Contact PCH Dental team urgently
- Replant ASAP: refer to Avulsion below
- If unable, store in Hank’s Balanced Salt Solution
|
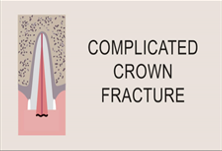
Tooth fractures
- Ascertain if the tooth is a primary or permanent tooth
- Most fractured teeth are highly sensitive to mechanical or thermal stimulation though not considered an emergency and can be managed in a routine clinical environment.
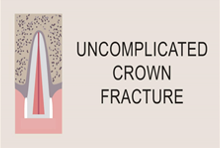
Uncomplicated crown fracture
Primary tooth
- Do not attempt to reposition, refer to a dentist.
- Further movement of the primary tooth may result in damage to the unerupted permanent tooth.
- An intrusion of up to 50% that is firm in position is often monitored for re-eruption over time and requires no immediate management.
Permanent tooth
The need to reposition an intruded permanent tooth is often determined by the stage of development of the tooth; requirement for treatment is generally associated with the onset of adolescence and will require urgent treatment by a staff dentist.
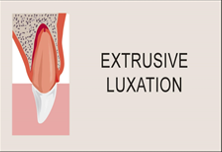
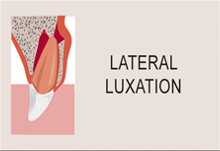
Luxation
- The tooth is moved from its normal position, the correct nomenclature indicating the direction of movement of the tooth crown (labial luxation, palatal luxation or extrusive luxation).
- The injury is usually associated with tearing of the gum margin and / or fracture of the alveolar bone.
- The tooth is usually loosened, but may be firm in an alveolar fracture.
Primary tooth
- Often requiring management under general anaesthesia for definitive treatment, luxated primary teeth are often monitored if they are stable in position and not interfering with closure of the jaw.
- Loose or malpositioned teeth that affect the bite require extraction.
Permanent tooth
- The majority of displaced permanent teeth will require repositioning and splinting.
- The success of treatment diminishes with the time elapsed since the injury, contact a dentist immediately.
Avulsion
- The tooth is completely dislodged from the socket, usually out of the mouth.
Primary tooth
- Never replant an avulsed primary tooth; this may damage the developing permanent tooth.
Permanent tooth
- Replant a permanent tooth back into the empty socket as soon as possible.
- Hank's Balanced Salt Solution (preferred) or milk are alternative storage media for avulsed teeth, but neither is as good as replanting the socket.
- Contact the on call dentist immediately from triage; do not await a medical consult first.
Management of an avulsed permanent tooth
- Pre-reimplantation prophylaxis is required only for patients where the consequences of transient bacteraemia are significant (e.g. previous bacterial endocarditis, immunosuppressive therapy, recently repaired cardiac defect). Administer antibiotic prophylaxis if required using a suitable dose of amoxicillin or clindamycin. Refer to Medical Prophylaxis guideline – Infective endocarditis prophylaxis for further information on applicable conditions, timing and dosage.
- Handle the tooth only by its crown, never touching the root surface.
- Administer an infiltration of local anaesthetic
- e.g. lidocaine 1% (50 mg / 5 mL) with adrenaline (epinephrine) 1:100,000 (50 microgram / 5 mL).
- Ensure tooth is clean and free of debris.
- If dirty, rinse for less than 10 seconds ideally in Hank’s Balanced Salt Solution or milk. Alternatively use sodium chloride 0.9% or where there is no alternative, plain water.
- Examine the socket: reposition socket wall if fractured, irrigate large blood clot with sodium chloride 0.9% or local anaesthetic.
- Replant tooth to most ideal position with fingers holding only the crown; reposition adjacent teeth if moved from position.
- Mould alveolar bone with fingers.
- Irrigate degloving injuries of mucosa and suture if margins are not well opposed.
- Temporarily stabilise replanted and repositioned teeth by moulding several layers of domestic aluminium foil extending at least 2 teeth either side of the repositioned teeth.
- Replanted teeth must be properly stabilised by the dental team as soon as possible to ensure favourable healing.
- Check tetanus immunisation status.
- Discharge with chlorhexidine 0.5% oral gel (Curasept Gel®), to be used twice daily for 1 week; advise a soft diet for 2 weeks.
- Discharge with oral antibiotics3:
- For children 8 years and older3:
- Oral doxycycline once daily for 7 days at appropriate dose for patient age and weight using the following dose bands:
- < 21 kg: 2.2 mg/kg once daily
- ≥ 21 to < 26 kg: 50 mg once daily
- ≥ 26 kg to < 35 kg: 75 mg once daily
- ≥ 35 kg: 100 mg once daily.
- If doxycycline is contraindicated or patient unable to swallow tablets: Oral amoxicillin 15 mg/kg/dose (to a maximum of 500 mg) 8-hourly for 7 days.
- Dental treatment is required as soon as possible to form a stable splint for the traumatised tooth, and to commence appropriate endodontic treatment.
- If unable to replant, store completely submerged in Hank’s Balanced Salt Solution or milk, alternatively wrap in cling wrap covered with patient’s saliva. Seek dental treatment as soon as possible.
Do not:
- Do not allow the tooth to dry out.
- Do not scrape the root surface.
- Do not rinse the tooth in water for a prolonged period.
- Do not store in ice.
- Do not store in water or sodium chloride 0.9%solution.
Soft tissue injury
- Gingival lacerations rarely require suturing.
- Most will heal perfectly well by themselves, or with simple measures such as lip taping. Gingival lacerations require suturing if there is:
- Significant tissue displacement
- Bone exposure
- Degloving of the maxilla or mandible
- Exposure of tooth roots
- Impaction of debris
- A requirement for haemostasis, or for other requirements.
References
- Textbook of Paediatric Emergency Medicine 3rd Edition Cameron P, Browne GJ, Mitra B, et al (2018) Publisher: Elsevier Edition updated
- Fleisher and Ludwig's Textbook of Pediatric Emergency Medicine Eighth Edition. Journal of Pediatric Critical Care 8.2 (2021): 116. Web. Kundan Mittal.
- Therapeutic Guidelines 2023. Oral & Dental: Tooth Avulsion. [Last Updated: March 2025. Cited: 05 June 2025] Available from: Topic | Therapeutic Guidelines (health.wa.gov.au)
| Endorsed by: |
Drugs & Therapeutics Committee |
Date: |
April 2025 |
This document can be made available in alternative formats on request for a person with a disability.