Fractures - Hand
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common-sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS Clinical disclaimer
|
See Fractures – Overview for General Assessment and Management
Mechanism of injury
- Distal phalanx tuft fractures are caused by crush injuries and often involve injury to the nail bed and nail plate.
- Avulsion fractures such as mallet finger and volar plate injuries are caused by hyperflexion or hyperextension of the finger.
- Phalangeal and metacarpal fractures are caused by direct trauma or rotational forces.
- Thumb ulnar collateral ligament injury (Gamekeeper’s thumb) is caused by hyper-abduction of the thumb.
Examination
- Compare both hands and look for bruising, erythema, swelling and deformity.
- Palpate for obvious areas of tenderness.
- Passive and active range of movement of all joints in hand and wrist should be examined. Testing against resistance may identify ligamentous injury.
- Assess for rotational deformity by asking the patient to make a fist. Look for “scissoring” or crossing over of the fingers.
- Assess for ulnar collateral ligament injury (Gamekeeper’s Thumb) by palpating for tenderness on the ulnar side at the base of the proximal phalanx and looking for pain / laxity on abduction of the thumb.
- Test sensation and motor function of the median, radial, and ulnar nerves.
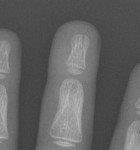
Imaging
- Request a finger X-ray if the injury is localised to one digit. This should have PA, oblique, and lateral views and include the metacarpal and carpometacarpal joint.
- A hand X-ray should have PA, oblique, and fan lateral views and will include all bones of the hand, carpus, and distal radio-ulnar joint.
Specific management
Complicated Hand and Finger Fractures
Refer any complicated fractures to the Plastic Surgery team.
- Open fractures
- Amputations
- Associated tendon injury
- Neurovascular compromise.
Resting Volar Slab
The resting volar slab can be used to immobilise most acute hand fractures. It is a position of safe immobilisation with minimal strain on hand ligaments.
- Plaster backslab on volar (palmar) aspect of hand and forearm.
- Wrist in 30º extension.
- Metacarpophalangeal (MCP) joints flexed to 60º – 90º.
- Inter-phalangeal (IP) joints at 180º (fingers fully extended).
Distal Phalanx Tuft Fractures
- Simple tuft fractures are managed with buddy strapping or aluminium splint with GP follow up.
- If associated pulp laceration, antibiotics may be required.
- If associated nail bed injury, refer to Plastic Surgery.
Mallet finger

Volar plate injury

- Dorsal blocking splint and follow up with plastic surgery clinic in 1-2 days
Other phalangeal fractures

Undisplaced extra-articular fractures with NO rotational deformity
- Buddy strap and resting volar slab with follow up in Plastic Surgery clinic in 1-2 days.
Displaced, angulated, intra-articular fractures or rotational deformity
- Reduce fracture under ring block +/- sedation if appropriate. Otherwise refer to the Plastic Surgery team.
- Buddy strap and resting volar slab with follow up in Plastic Surgery clinic in 1-2 days.
Finger amputations

- All finger amputations should be referred urgently to Plastic Surgery.
- Irrigate stump with sodium chloride 0.9% and cover with sodium chloride 0.9% soaked gauze.
- Irrigate amputated part with sodium chloride 0.9%, wrap in sodium chloride 0.9% soaked gauze, place in a watertight plastic bag, and place the closed bag in an ice slurry.
- Treat as an open fracture (nil by mouth, intravenous antibiotics, tetanus booster if required).
Metacarpal fractures (2nd to 5th)

Undisplaced extra-articular fractures with NO rotational deformity
- Resting volar slab and follow up with Plastic Surgery clinic in 1-2 days.

Displaced, angulated, intra-articular fractures or rotational deformity
- Most common is 5th "Boxer's Fracture".
- Reduce fracture under nerve block +/- sedation if appropriate. Otherwise refer to Plastic Surgery team.
- Resting volar slab and follow up with Plastic Surgery clinic in 1-2 days.
Thumb Fractures
Undisplaced extra-articular fractures

- Thumb spica cast and follow up with Plastic Surgery clinic in 1-2 days.
Displaced, angulated, or intra-articular fractures

- Reduce fracture under ring block +/- sedation if appropriate. Otherwise refer to Plastic Surgery team.
- Thumb spica cast and follow up with Plastic Surgery clinic in 1-2 days.
Suspected ulnar collateral ligament injury (Gamekeeper’s Thumb)
- Thumb spica cast and follow up with Plastic Surgery clinic in 1-2 days.
1st Metacarpal Fractures
Undisplaced extra-articular fractures
- Thumb spica cast with follow up in Plastic Surgery clinic in 1-2 days.
Displaced, angulated, or intra-articular fractures
- Reduce fracture under ring block +/- sedation if appropriate. Otherwise refer to Plastic Surgery team.
- Thumb spica cast and follow up with Plastic Surgery clinic in 1-2 days.
References
- Andrade A, Hern HG. Traumatic Hand Injuries: The Emergency Clinician’s Evidence Based Approach. Emergency Medicine Practice. 2011; 13(6)
- McRae R, Max Esser M, Practical Fracture Treatment Fifth Edition, Churchill Livingstone, 2008
- Rang M, Pring ME, Wenger DR. Kluwer W, Rang's Children's Fractures Fourth edition. Wolters Kluwer, 2018
- Yeh PC, Dodds SD. Pediatric Hand Fractures. Techniques in Orthopedics. 2009; 24(3): 150-162
| Endorsed by: |
Nurse Co-Director, Surgical Services |
Date: |
Feb 2024 |
This document can be made available in alternative formats on request for a person with a disability.