Observation, Monitoring and Paediatric Acute Recognition and Response Observation Tool (PARROT)
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Aim
To outline the minimum requirements for assessment, observation, non-invasive cardiorespiratory monitoring, and documentation of clinical observation using the Paediatric Acute Recognition and Response Observation Tool (PARROT).
Background
Early recognition of deterioration, followed by prompt and effective action, can reduce adverse outcomes and minimise interventions required to stabilise patients who deteriorate in hospital.1
Effective management of acute deterioration requires accurate measurement, recognition and interpretation of abnormal clinical observations followed by appropriate escalation of care.2
Track and trigger systems are formal processes that rely on measurements of observations (tracking) with predetermined escalation criteria (trigger) when certain thresholds are met.2 PCH uses an ESCALATION system to recognise and respond to clinical deterioration which includes:
- the PARROT
- the Early Warning Score Escalation Pathway
- Paediatric Sepsis Pathway Trigger
- CARE Call
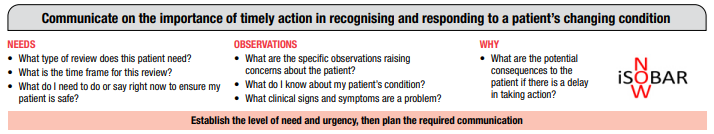
- a structured communication tool (iSoBAR).3
Key points
- This procedure outlines the minimum standards for patient observation and monitoring based on the best available evidence. It is not intended to replace more comprehensive education or clinical judgement.
- Patients at PCH must have observations, assessment, and monitoring appropriate to their clinical situation documented at a frequency that is appropriate to optimising recognition of acute deterioration.
- The patient’s observations, assessment and monitoring requirements are to be clearly documented and communicated among members of the healthcare team.
- Documentation of clinical observations must be recorded on the age-appropriate PARROT Chart (exceptions include Paediatric Critical Care; Neonatal Intensive Care Unit and Theatre / Medical Imaging).
- Identified acute deterioration or significant changes in clinical observations must be reported immediately to the treating team and escalated in accordance with the Early Warning Score Escalation Pathway or Paediatric Sepsis Pathway Trigger, STARS - Safety Team After-hours Response Service and Resuscitation and Responding to Clinical Deterioration. MET Review and Code Blue procedures (internal WA Health only).
- Patients receiving palliative care or who are at the end of life may not require their core vital signs to be monitored but require monitoring of symptoms associated with Paediatric Goals of Patient Care (PGoPC) (internal WA Health only). This plan must be clearly documented, including alterations to escalation processes.
- Clinical observations are not to be recorded on the MR 868.08 PARROT Clinical Comments Chart but may be used to supplement documentation of additional findings in conjunction with the PARROT.
- When transitioning a patient from a specialty area to a general clinical setting a PARROT is to be commenced prior to transfer to allow for continuation of clinical observation trend monitoring.
- Clinical assessment of the paediatric patient is a continuous and dynamic process. Singular assessments may immediately identify deterioration, however repeated observations over time are often required to ensure subtle signs or cues of illness are detected.1 Due to compensatory measures, clinical severity may be greater than it appears.3 Normal vital sign parameters do not guarantee a stable physiological status.
- Clinical observations must be considered in relation to each other and the full clinical picture.3
- Clinical judgement is paramount. If CONCERNED about the patient, call for immediate medical assistance via Medical Emergency Team (MET) or Code Blue (internal WA Health only).
Observation and monitoring plan
- A monitoring plan outlines the minimum observation and assessment requirements for a patient in the acute care setting and should be developed with consideration of the patient’s diagnosis and proposed treatment. This may be an individualised plan documented in the nursing care plan and / or patient record or specified in a clinical pathway or guideline for a cohort of patients.2
- The monitoring plan must specify the minimum:
- Clinical observations to be recorded.
- Frequency of assessment.
- Duration of the plan (where applicable).
- The monitoring plan must be documented in the patient medical record on admission and reviewed at least daily, and whenever there is a change in the patient’s clinical condition.
- Frequency of observations should only be decreased in consultation with the Shift Coordinator, a Clinical Nurse or the treating medical team.
- Increased frequency of observations can be initiated by nursing staff based on clinical judgement of a patient’s condition or as specified in the escalation plan.
- Monitoring plans should be in according with the ACSQHC National Consensus Statement: Essential Elements for Recognising and Responding to Acute Physiological Deterioration2
- Patients’ vital signs should be measured at the time of initial assessment, on admission and when a patient moves between areas within a hospital and across the health system
- The frequency of observations should be consistent with the clinical situation of the patient. For the majority of patients in a health service organisation, vital signs should be measured at least every 6 hours.2
- At a minimum, hourly respiratory assessment and documentation of vital signs must be undertaken for all patients requiring acute oxygen therapy or who have an acute respiratory illness. Refer to the section below on Respiratory Rate and Respiratory Distress Assessment.
- For patients’ post-surgery, the observation and monitoring plan may be specific to the procedures undertaken. Refer to the post-operative instructions and to Post Operative Care guideline (internal WA Health only).
Skills and equipment1
- Medical and nursing staff have access to education and resources which support accurate measurement and interpretation of vital signs, including the clinical significance of acceptable and abnormal vital signs in the context of acute paediatric physiological deterioration.
- All staff and students will undertake clinical observations including vital signs according to their education, training and scope of practice and where required, under the supervision of skilled staff.
- Accurate measurement is dependent on correct use of equipment. Ensure that equipment for measuring and monitoring vital signs and other physiological parameters is readily available, in good working order, and is used in accordance with the manufacturer’s instructions.
- Alarm limits should be set by selecting the appropriate age-related profile on the monitor. Subsequent adjustment of the alarms may be required, however should be made with caution. It may be necessary to set the alarm limits within a narrower range for some patients. The key principle is to provide safe alarm settings for the child whilst minimising false alarms.
- All alarms must be 'enabled' (activated) and audible from the staff base.
- When an alarm sounds clinicians should respond immediately to assess the child and enact the appropriate intervention / response system as required.
- Parents / visitors are not permitted to disable alarms or alter alarm settings.
Indications for continuous monitoring
- Continuous monitoring complements intermittent clinical observation by alerting clinicians to rapid changes in a patient’s condition.
- Some patients will require continuous monitoring as a management requirement related to their specific condition, intervention or treatment (refer to Related CAHS internal policies, procedures and guidelines). In addition, all patients who are either clinically unstable, or at risk of sudden changes in their condition, should be continuously monitored by the most appropriate method, especially overnight or if unsupervised.
- Continuous monitoring can refer to any of the three types listed below. Monitoring plans and clinical guidelines that recommend continuous monitoring must specify which of these is required:
- Pulse oximetry monitoring
- Cardiac monitoring (3 lead echocardiogram (ECG))
- Respiratory rate and apnoea monitoring (e.g. infant monitoring criteria – see Post Operative Care – internal WA Health only)
- Patients with acute respiratory distress, acute oxygen therapy, or any potential for hypoxaemia and/or airway restriction or obstruction are to be continuously monitored with pulse oximetry and/or apnoea monitoring. This includes patients with seizure disorders, particularly overnight, if unsupervised or if clinically unstable.
- Patients with a risk of arrhythmia are to be monitored continuously with 3-lead ECG at a minimum.
- Identification of arrhythmia on ECG is an advanced nursing skill. Patients requiring continuous ECG monitoring should be managed in clinical areas with staff that are trained and skilled.
Continuous electrocardiographic (ECG) monitoring6,8
- Standard placement of the 3 electrodes for continuous ECG monitoring:
- Apply RA electrode (white) directly below the clavicle and near the right shoulder.
- Apply LA (black) electrode directly below the clavicle and near the left shoulder.
- Apply LL (red/green) electrode on left iliac fossa (left lower abdomen).
- Set the monitor to appropriate ECG lead either, I, II, III.
- Lead II is the preferred lead, as it most closely resembles the normal pathway of current of flow in the heart and therefore displays an upright complex with an optimal signal.
- ECG electrodes should adhere tightly to the patient’s skin to prevent external influences from affecting the ECG trace. Check the skin regularly for reaction to electrode adhesive.
- ECG electrode placement should be checked each shift as accurate interpretation of arrhythmias depends on proper placement of electrodes and knowing which lead is being viewed.
- If an arrhythmia is detected, immediately assess the patient, initiate appropriate medical care and request a prompt medical review. If concerned about the patient, place a MET call or Code Blue.
PARROT instructions for use
General instructions
- The PARROT has a suite of 5 age-specific tools: Selection of the correct age chart is crucial (patients actual age, do not adjust for corrected gestational age). This allows for identifying deviation from the acceptable age-defined parameters indicated on the chart.
- Less than 3 months
- 3-12 months
- 1-4 years,
- 5-11 years and
- 12 years and above.
- Calculation of an early warning score requires all 10 values on the chart to be assessed, documented, and summed as a total early warning score.
- Calculation and documentation of a total early warning score is to be undertaken at a minimum:
- For all patients on presentation and admission
- After a transfer from another ward / clinical area including after the child has undergone a procedure
- When any of the clinical observations move into a higher-scoring shaded area (a change from previous observations)
- If there is any clinical indication that the patient may be deteriorating
- If a clinician is concerned about the patient’s clinical condition
- If the parent / carer expresses concern about the child’s condition. The parent / carer should be asked at each assessment how they feel their child is progressing (refer to Aishwarya’s CARE Call: Family Escalation policy – internal WA Health only).
- Abnormal clinical observations must be closely monitored until they return to the acceptable parameter range.
- All observations within the range indicated on the chart must be recorded graphically to support identification of subtle trends. Exceptions to this are outlined below. Refer to Modifications section below.
- If the patient’s clinical observation falls on the line between two differently scoring zones, the early warning score is calculated using the higher score.
- Any clinical observations outside the acceptable range indicated on the chart must be written as a number in the designated space for numeric values for the relevant clinical observation.
- The clinical observations recorded in the PARROT are presented in an Airway, Breathing, Circulation, Disability, Exposure (ABCDE) format to reflect APLS training and clinical priority.
Escalation
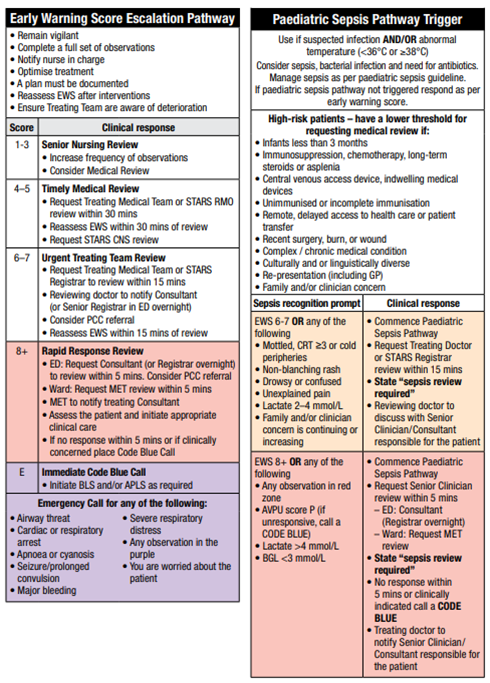
- The Early Warning Score Escalation Pathway prompts appropriate intervention and escalation according to the patient’s total early warning score. The Paediatric Sepsis Pathway Trigger prompts recognition of sepsis and criteria for a sepsis review. (refer to Appendix 1: Escalation Pathways below and refer to Sepsis recognition and management guideline).
- Interventions / actions in response to clinical deterioration or concern are to be documented on the front of the chart and referenced with the corresponding clinical observations assessment. A more detailed description of the event, escalation and response should be recorded contemporaneously in the patient’s medical record.
- Initiate a higher level of escalation if unable to achieve review within the specified response time, or if there are concerns a delay may lead to further deterioration.
- Concerned parents / carers can initiate medical review when they are concerned their child’s condition is worsening and do not feel there has been adequate response, in accordance with the Aishwarya’s CARE Call: Family Escalation process – internal WA Health only.
- Calculate and document a total early warning score as clinically indicated or within half an hour of the intervention / escalation to assess effectiveness and the need for any further action.
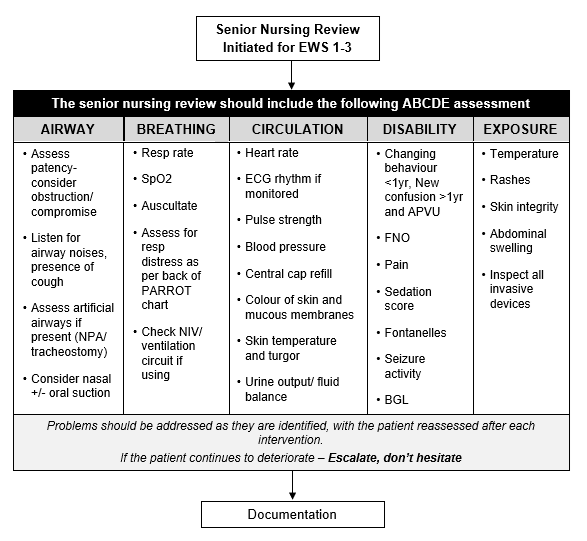
- A Senior Nursing Review can be conducted by a registered nurse in roles such as Shift Coordinator, Clinical Nurse Manager, Liaison Nurse, Staff Development Nurse or Senior Registered Nurse.
- The senior nurse will apply their clinical judgement after they are asked to review a patient. This assessment may include any or all elements of the ‘Decision making flowchart for a Senior Nursing Review’ Refer to Appendix 2: Decision making flowchart for a Senior Nursing Review – below).
- The Senior Nursing Review must be documented in the patient’s medical notes, including assessment, interventions, need for further escalation and ongoing monitoring plan. Use iSoBAR NOW when escalating clinical concerns / clinical deterioration.
Modifications
- Some patients will have expected abnormal clinical observations which are not necessarily indicative of the need for escalation of care. These may be due to chronic illness, treatment regimens or clinical diagnosis. In these circumstances a modification to the patient’s acceptable parameters may be considered and documented on the PARROT in line with the below requirements.
- Modifications to acceptable clinical observation parameters are to be made with caution, especially in the context of acute illness.
- Modifications must be reviewed regularly, as per the patient’s needs.
- Minimum standards are for 72 hourly review; however this should ideally be more frequent (at least every 24 hours).
- Modifications must NOT be used to normalise a clinically unstable patient.
- The reason for the modification must be documented in the modification section of the PARROT.
- Modifications should not be put in place for assessment of Level of Consciousness, this includes AVPU, UMSS, changing behaviour or new confusion.
- Modifications must only be made by, or in consultation with, the child’s primary treating team.
- Consultants are the preferred personnel to document modifications.
- RMOs and Registrars can only document modifications after a discussion with the Consultant has occurred and has been documented.
- Medical staff documenting modifications on the PARROT must also record in the patient’s medical record and include:
- A monitoring and modified escalation plan for the patient.
- A timeframe for the modifications (≤72 hours).6
- Modifications must not be transcribed to new charts by nursing staff. If a new chart is commenced, modifications must be reviewed and documented by medical staff as above.
- Documentation and escalation when modifications are in place:
- Observations are still recorded on the PARROT, and when applicable the total early warning score is still calculated as per standard practice (excluding the value of the modified clinical observation).
- The early warning score, the modification parameter and clinical judgement must all be considered when selecting the appropriate action. To calculate the revised score, the parameter to which the modification is applied would be omitted from the calculation.
- For example: a patient has a total early warning score of 8 (MET criteria) and a modification is documented for a parameter that was scoring a 2, that ‘2’ is omitted from the calculation and the revised Early Warning Score would be 6.
- Document on the chart as a score of 6 and note in the events section that the escalation has been revised (as per the modifications) to a Registrar Review. However, if the nurse (or family/carer) holds clinical concern for the patient, they may choose to take the higher course of escalation.
- Should the patient’s observation later exceed the modified parameter, apply the score as per the chart, include it in the calculation of the Early Warning Score and follow the relevant Escalation Pathway.
- Clinical judgement should not be overridden by documented modifications.
PARROT clinical comments sheet
- The MR 868.08 PARROT Clinical Comments Chart is only to be used for brief documented comments that provide additional information directly related to clinical observation assessment at the corresponding time. Examples of appropriate use include:
- Chest sounds on auscultation when assessing respiratory distress.
- Pulse quality on palpation when assessing heart rate.
- Do not record clinical observations on the Clinical Comments Sheet. All clinical observations (including fleeting changes and those seen on monitors from the staff base) must be recorded contemporaneously on the PARROT.
- Do not record actions or interventions on the MR 868.08 PARROT Clinical Comments Chart. These must be recorded on the PARROT interventions section with more detailed documentation in the inpatient progress notes.
Transition from speciality area to a general ward
Post Anaesthetic Care Unit (PACU)
- When patients reach the PACU discharge criteria, a full set of observations must be completed, a total early warning score calculated and documented on a PARROT.
- If the total early warning score is ≥4, the patient is to be reviewed by the anaesthetist.
Critical care areas
- PCC / High Dependency Unit (HDU) & Neonatal Intensive Care Unit (NICU)).
- When patients in these areas are ready for discharge a copy of the PCC / HDU or NICU observation chart will go with the patient, and the receiving nurse will complete a full set of observations on the PARROT on admission to the ward.
Documenting observations on the PARROT chart
- All observations, except blood pressure, are to be recorded as linear graphs; dots recorded in the graphical areas must be connected with a straight line. Recording observations as linear graphs assists in recognising trends and is in line with the ASQHC’s Consensus Statement.1,2
- Graphical areas of the chart are for the recording of linear graphs only and must be kept free of text. Any additional comments about observations should be recorded as an event on the front on the PARROT and/or in clinical comments.
- See example in Appendix 3: Example of recording observations on the PARROT for how to record all clinical observations on the PARROT – below.
Family or clinician concern variable
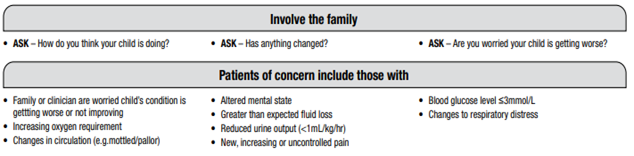
- Family or caregiver concern is highly predictive of paediatric patient deterioration.7 Concern about clinical deterioration can be indicated by the family or caregiver and/or clinician and is measured as a weighted variable when undertaking clinical observations. This is in recognition of the early subtle signs of clinical deterioration which can be detected by families and staff.
- ‘Clinician’ refers to medical, nursing or allied health professional who may be concerned about the patient.
- Where possible parents / carers and the child should be actively included in any assessment using the PARROT tool and parents/carers asked if they have any concerns about their child’s condition.
- Record family / clinician concern graphically as connected dots.
- When family and/or clinician concern is present, this must be documented as an event and/or in the clinical notes.
Airway and breathing
Assessment of respiratory distress, respiratory rate and SpO2
- At a minimum, hourly respiratory assessment, monitoring and documentation of clinical observations must be undertaken for all patients requiring acute oxygen therapy or who are acutely unwell with a respiratory illness.
- Respiration rate should be counted manually for a period of 60 seconds.
- Apnoea is defined as no respiratory effort for a period of more than 20 seconds or no respiratory efforts for 10 seconds if accompanied by bradycardia, oxygen desaturation or cyanosis.20 A brief apnoea is described as 5-10 secs and prolonged apnoea >20 seconds.12,13
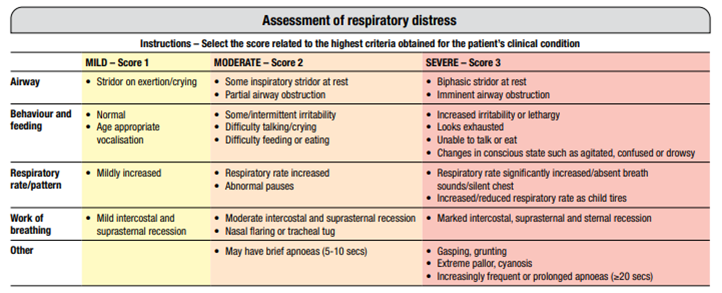
- Assessment of respiratory distress is completed using a standardised assessment tool which has four levels: nil, mild, moderate or severe.
- Record assessment of respiratory distress graphically as connected dots.
Respiratory rate
- Record respiratory rate graphically as connected dots.
Oxygen saturations (SpO2)
- SpO2 is an indirect measurement of arterial oxygen saturation using a pulse-oximeter.
- SpO2 is recorded numerically as a percentage (%) on the PARROT Chart.
- Factors that can affect accuracy of SpO2 reading include:
- Incorrect choice of probe for age / size
- Poor positioning
- Probe secured too tightly,
- Poor perfusion or significant hypothermia
- Synthetic fingernails / dark nail varnish
- Excessive ambient light
- Motion artefact
- Probe or monitor malfunction.
- For patient’s requiring continuous pulse-oximetry, skin integrity at the probe site should be checked with each set of observations and the probe site rotated every 2 to 4 hours, more frequently for patients at increased risk of pressure injury (e.g. neonate/infant). Probe change is to be recorded on the PARROT.
- Saturation probe should not be left in place if continuous monitoring is not required.
- Pulse-oximeter should not be used as a substitute for palpation to obtain heart rate.
- Record oxygen saturations graphically as connected dots. Oxygen Therapy and Mode of Delivery
- Patients requiring acute oxygen therapy are to have respiratory assessment undertaken and recorded on the PARROT hourly at a minimum, or more frequently as indicated by their clinical status and / or monitoring plan.
- Respiration rate; respiratory distress; oxygen saturations
- Oxygen flow rate; mode of delivery
- Heart rate.
- Refer to the relevant guidelines for detailed information on indications, specific assessment requirements, recording of additional observations (e.g. equipment function checks), medical review, oxygen delivery devices and weaning, e.g.
- Oxygen Administration
- Humidified High Flow Oxygen Therapy (HHF)
- Non-Invasive Ventilation
- Bubble CPAP (Continuous Positive Airway Pressure)
- Record oxygen flow (L/min) or percentage (%) of oxygen being administered at time of assessment in the space allocated for mode of oxygen delivery.
- Oxygen therapy should also be recorded graphically with connected dots.
- Use the following key to indicate mode of oxygen delivery.
|
BCPAP
|
Bubble CPAP
|
|
BiPAP
|
Bilevel positive airway pressure
|
|
C
|
Continuous positive airway pressure (CPAP)
|
|
FM
|
Face Mask
|
|
HHF
|
Humidified High Flow
|
|
HME
|
Heat and Moisture Exchanger (Swedish nose)
|
|
NP
|
Nasal Prongs
|
|
NRM
|
Non Re-Breather Mask
|
|
RA
|
Room Air
|
|
T
|
Tracheostomy
|
|
VENT
|
Any other form of assisted ventilation
|
|
WO
|
Wafting Oxygen
|
Circulation
Heart rate (pulse)
- The heart rate should be counted for one full minute noting the rate, depth and rhythm by palpation of the pulsation or consider using a stethoscope over the apex of the heart if required for:
- Patients under 2 years
- Patients with cardiac problems
- Irregular pulse on palpation2
- If assessing pulse using a stethoscope, pulse volume must also be assessed by palpation.2
- Record heart rate graphically as connected dots.
Blood pressure
- Blood pressure (BP) should be recorded using a connected ‘v’ and inverted ‘v’ notations. The diastolic value and pulse pressure must be clinically considered, however only the systolic reading is included in the early warning score.
- The upper arm is the preferred site for measurement and should be supported and positioned at heart level. If the arm is not suitable for cuff placement, the calf may be considered.
- Incorrect cuff size and fitting can lead to inaccurate readings. The cuff bladder should cover 80-100% of the chosen limb’s circumference. Position the centre of the leads over the artery. Cuff should cover a minimum of 40% of the length between shoulder and elbow.
- Inaccurate BP may be obtained if the child is crying or if the leads or cuff inflation is impeded. Abnormal blood pressures should be repeated for accuracy
- If an abnormal blood pressure is detected by an automated machine, it should be confirmed by a manual BP to avoid misdiagnosis and incorrect treatment. Obtaining a manual BP should not delay escalation of care14
- Hypotension is a late and pre-terminal sign of circulatory failure and should be reported to the treating medical team, +/- MET/code blue.
- Hypertension can be a sign of renal, cardiac or endocrine issues and a sign of raised Intracranial Pressure (ICP) and should be escalated appropriately.2
Postural blood pressure
- Position the patient supine and or as flat as clinically permitted for 10 minutes prior to the initial measurement of blood pressure and pulse. Record BP and Heart Rate (HR) measurements on the PARROT and write ‘Lying’ in the white box below the BP.
- Sit or stand the patient upright and repeat the BP and HR after 1 minute and record on the PARROT and write ‘Standing’ in the white box below the BP.
Capillary refill time (central)15
- Exert cutaneous pressure (sufficient pressure to blanch skin) on the centre of the sternum for 5 seconds. Release pressure and count in seconds how long it takes for the skin to return to its original colour.
- A delay in capillary refill time is a warning sign for haemodynamic compromise and should be reported as per the Early Warning Score Escalation Pathway and to the treating medical team.
- Record central capillary refill time graphically as connected dots.
Disability
Pain assessment
- Age-appropriate pain assessment tools are provided on the back of the correct aged PARROT.
- A pain score should be recorded with every set of clinical observations.
- Unexplained pain or increasing or uncontrolled pain are signs of potential clinical deterioration and possible sepsis.
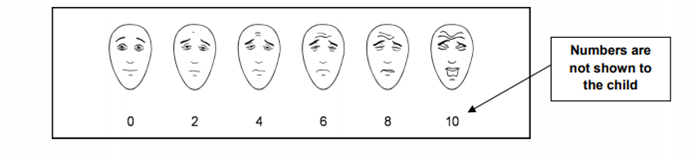
- The 3 pain scales used are the Face, Legs, Activity, Cry and Consolability Pain Scale (FLACC), the Faces Pain Scale – Revised (FPS-R) and the Numerical Rating Scale (NRS).
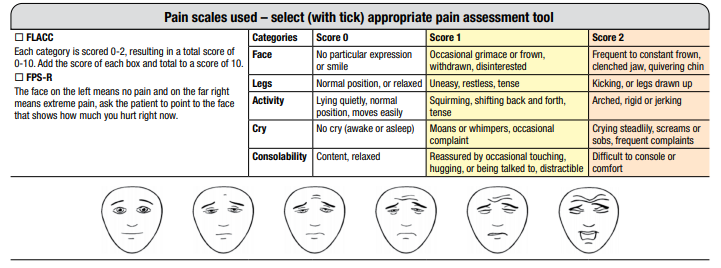
- The corresponding pain scores for the FPS-R are not listed on the PARROT so it can be shown to patients (numbers are not shown to the child). Below are the corresponding scores for the scale beginning at 0 and progressing at increments of 2 up to a maximum score of 10.
- If the patient is requiring an opioid or regional infusion, the pain score must be recorded on both the Pain Assessment and Management Record (MR871) and the PARROT.
- Record pain score graphically as connected dots.
Level of consciousness2,10
- For patients with specific neurological concerns, a more comprehensive neurological assessment, which is documented on the age-appropriate Neurological Observation Chart, is to be performed as per Neurological Observations (internal WA Health only). The use of a Neurological Observation Chart should be considered for any patient who has, or has the potential, to have an altered neurological state.
- For all other patients, assess the child’s level of consciousness by assessing new confusion (assessed in patients > 1 year), changing behaviour (assessed in patients < 1 year) as well as Alert, Voice, Pain, Unresponsive (AVPU) or if sedation has been administered the University of Michigan Sedation Scale (UMSS) is to be used (see next section for more information on UMSS).
- If a patient is receiving procedural sedation, the new variables of changing behaviour and new confusion cannot be assessed. UMSS should be used to assess consciousness.
- Changing behaviour / New confusion assessment is done in context of the patient’s developmental age and/or baseline assessment, noting changes in cognitive function, activity/tone, perception, or emotional state such as abnormal thinking, irritability, agitation, inconsolability and/or delirium.15
- For further information about delirium refer to the CAHS Policy on Recognising and Responding to Acute Deterioration and the PCH PCC policy on Delirium Assessment and Management (internal WA Health only).
- New confusion, changing behaviour, or changes in conscious level can be due to a variety of reasons including infection, hypotension, hypercapnia, hypoxia, side effects of medication, electrolyte imbalances, neurological conditions, pain, withdrawal syndromes and delirium.15,16
- Changing behaviour / new confusion and AVPU are recorded as separate variables and are scored independently (refer to example chart in Appendix 3: Example of recording observations on the PARROT– below).
- Level of activity can be used to assess infants < 3 months.
- The child must be awake in order to assess Level of Consciousness. If necessary, wake patient before scoring.
- Any deterioration in neurological status should trigger a full Neurological Observations assessment and medical review11
- Painful central stimulus can be delivered by squeezing the trapezius or sternal pressure.2
- Record new confusion (assessed in patients > 1 year), changing behaviour (assessed in patients < 1 year) and AVPU graphically as connected dots.
- Record new confusion (assessed in patients > 1 year), changing behaviour (assessed in patients < 1 year) and AVPU graphically as connected dots.
- If patient has prolonged/unresolved behaviour change or ongoing confusion, staff should escalate as per EWS and notify the shift coordinator and primary team to ensure a monitoring plan is put in place.
- The monitoring plan must be documented in patient medical record on admission and reviewed daily, and whenever there is a change in patient’s clinical condition
- Frequency and duration for the variable ‘changing behaviour/new confusion’ can only be completed by the treating medical team/ Senior Registrar/Consultant
Assessing changing behaviour / New confusion on the PARROT chart
|
Changing behaviour
(assessed in patients < 1 year)
|
3
|
Changing behaviour. Refers to a noticeable deviation from an infant's typical patterns of action, expression, or response.
Examples of Changing behaviour in an infant may include (but not limited to):16,17
- Not making eye contact with caregiver
- Underactive or hyperactive when awake
- Less than usual words / vocal sounds
- Inconsolable / irritable cry
- Restless
- Reflex present/absent or abnormal
- Disruptive sleep pattern
|
|
New confusion
(assessed in patients > 1 year)
|
3
|
New confusion. Refers to new onset disorientation, or cognitive impairment, where previously their mental state was normal for their developmental age – this may be subtle. The patient may respond to questions coherently, but there is some confusion, disorientation and/or agitation.
Examples of New confusion may include (but not limited to):16,17,18.
- Disorientation
- Reduced awareness
- Disorganised thinking
- Reduced or disrupted sleep patterns
- Non purposeful actions (e.g., repetitive movements)
- Impaired speech
- Agitated, inconsolable, or restless
|
Assessing AVPU on the PARROT chart
|
A
|
0
|
Alert. The patient is alert and interactive.
If the patient is acutely confused, a Glasgow Coma Score must be obtained, and the Early Warning Score Escalation Pathway should be followed.
|
|
V
|
1
|
Voice. The patient responds to voice.
If the patient is abnormally drowsy assess the patients Glasgow Coma Score (GCS). If this is a sudden change in conscious state activate a MET Review or CODE BLUE
|
|
P
|
3
|
Pain. The patient responds only to central pain.
If the patient responds only to pain, assess the patients Glasgow Coma Score (GCS) and reassess regularly. If this is a sudden change in neurological status, then activate a MET Review or CODE BLUE immediately.
|
|
U
|
E
|
Unresponsive. The patient is unresponsive.
A CODE BLUE must be activated.
A Glasgow Coma Score must be obtained.
|
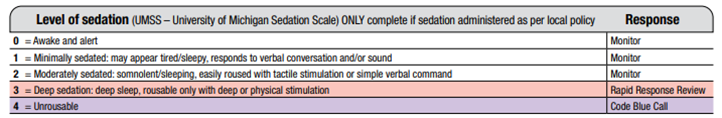
Level of sedation
- The University of Michigan Sedation Scale (UMSS) provides a more sensitive indicator of sedation than AVPU in sedated patients.
- The UMSS should be used when administering medications with sedative effects including procedural sedation and opioid analgesics. Refer to the Procedural Sedation guideline (internal WA Health only) and specific medication monographs for further instruction.
- AVPU scale and assessment of changing behaviour and new confusion can be reinstated once the patient has recovered from the sedative effects of the medications used.
Glucose level (BGL)
- BGL should be checked whenever there is seizure, (if clinically indicated) change in level of consciousness, suspected sepsis or concern about glucose levels.
- Record blood glucose level as a numeric value in white box.
- Known or suspected diabetic, metabolic or endocrine condition.
- Ability to record BGL in the PARROT does not replace the relevant PCH insulin chart for diabetes patients.
Temperature
- Digital axilla and tympanic thermometers are used at PCH. Accurate measurement is reliant on correct use of the thermometer in accordance with the manufacturer’s instructions.
- Axilla temperature measurement is preferred in infants and children from birth to five years of age.19
- Tympanic thermometers are not recommended for use in patients with known ear infections or when excessive ear wax is present.
- Record temperature graphically as connected dots.
Appendix 1: Escalation pathways
Appendix 2: Decision making flowchart for a Senior Nursing Review

References
- Australian Commission on Safety and Quality in Health Care. National Safety and Quality Health Service Standards. 2 ed. Sydney NSW: Australian Commission on Safety and Quality in Health Care; 2021.
- Australian Commission on Safety and Quality in Health Care. National Consensus Statement: Essential elements for recognising and responding to acute physiological deterioration. 3 ed. Sydney, NSW: Australian Commission on Safety and Quality in Health Care; 2021.
- Gill FJ, Cooper A, Falconer P, Stokes S, Leslie GD. Development of an evidence-based ESCALATION system for recognition and response to paediatric clinical deterioration. Aust Crit Care. 2022;35(6):668-76.
- Government of Western Australia. Recognising and Responding to Acute Deterioration Policy. Department of Health; 2023.
- Anna McCorquodale, Tessa Davis. Approaching the paediatric ECG, Don't Forget the Bubbles 2024. Available from: https://dontforgetthebubbles.com/approaching-the-paediatric-ecg/
- Ed Burns, Robert Buttner. Life in the Fast Lane: Paediatric ECG Basics 2024. Available from: https://litfl.com/paediatric-ecg-basics/
- Gill F, Boyle E, Adama E, Zhou J, Laird P, Harris T, et al. Improving assessment for paediatric clinical deterioration through the escalation system integrated family involvement. Australian Critical Care. 2024;37(5).
- Royal College of Nursing. Standards for Assessing, Measuring and Monitoring Vital Signs in Infants, Children and Young People: Clinical Professional Resource. London, UK: Royal College of Nursing; 2017.
- Kondamudi NP, Khetarpal S. Apnea in Children. StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
- Noah P. Kondamudi, Lewis Krata, Andrew S. Wilt. Infant Apnea. Treasure Island, Florida: StatPearls Publishing; 2023.
- Advanced Life Support Group. Advanced Paediatric Life Support: A Practical Approach to Emergencies. 7 ed. West Sussex, UK: John Wiley & Sons Ltd.; 2023.
- Parker G, Thakker P, Whitehouse WP. Evaluation of the child with syncope. Paediatrics and Child Health. 2016;26(5):219-24.
- Royal College of Nursing. Standards for assessing, measuring and monitoring vital signs in infants, children and young persons. [Expert opinion] 2017 5 May 2014. Available from: https://www.rcn.org.uk/professional-development/publications/pub-005942
- The Sydney Children’s Hospital Network. Guideline: Between the Flags – Clinical Emergency Response System (CERS). 2022. Available from: Recognition and management of patients who are deteriorating
- Harris J, Ramelet A, van Dijk M, et al. Clinical recommendations for pain, sedation, withdrawal and delirium assessment in critically ill infants and children: An ESPNIC position statement for healthcare professionals. Intensive Care Medicine. 2016;42:972-86.
- The Royal Children’s Hospital Melbourne. Guideline: Altered conscious state. [Internet]. Retrieved 2025 Feb 4. Available from Clinical Practice Guidelines: Altered conscious state (rch.org.au)
- Silver G, Kearney J, Traube C, Hertzig M. Delirium screening anchored in child development: the Cornell Assessment for Pediatric Delirium. Palliat Support Care. 2015 Aug;13(4):1005-11. doi: 10.1017/S1478951514000947. Epub 2014 Aug 15. PMID: 25127028; PMCID: PMC5031084.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5-TR. 5th ed. Arlington (VA): American Psychiatric Association Publishing; 2022.
- Ward, M. Fever in infants and children: pathophysiology and management [Internet]. UpToDate. [cited 2025 Feb 4]. Available at Fever in infants and children: Pathophysiology and management - UpToDate (health.wa.gov.au)
- Kondamudi NP, Khetarpal S. Apnea in children. [Updated 2023 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441894/
| Approved by: |
Clinical Practice Advisory Committee |
Date: |
Nov 2025 |
| Endorsed by: |
Co-Director Surgical Services (Nursing) |
Date: |
Nov 2025 |
This document can be made available in alternative formats on request for people with disability.