Head shape and size abnormalities
Disclaimer
These guidelines have been produced to guide clinical decision making for the medical, nursing and allied health staff of Perth Children’s Hospital. They are not strict protocols, and they do not replace the judgement of a senior clinician. Clinical common sense should be applied at all times. These clinical guidelines should never be relied on as a substitute for proper assessment with respect to the particular circumstances of each case and the needs of each patient. Clinicians should also consider the local skill level available and their local area policies before following any guideline.
Read the full CAHS clinical disclaimer.
|
Please discuss with the on call General Paediatric Team if:
- Bulging fontanelle
- Abnormal eye movements
- Excessive vomiting, sleepiness, irritability, seizures
Introduction
Variation in head shape and size is common.
Positional/Deformational Plagiocephaly
- Very common and results from moulding forces (such as position in utero, lying in the same position) on the developing skull. The typical features are an asymmetrical head shape with flattening on one side of the occiput. The ear, cheek and forehead may be pushed forward on the flattened side. Head shape resembles a parallelogram when viewed from above - the nose is straight, and the ears are aligned in the transverse plane. Positional plagiocephaly is a cosmetic condition. It does not affect brain growth or development and will generally resolve with conservative management.
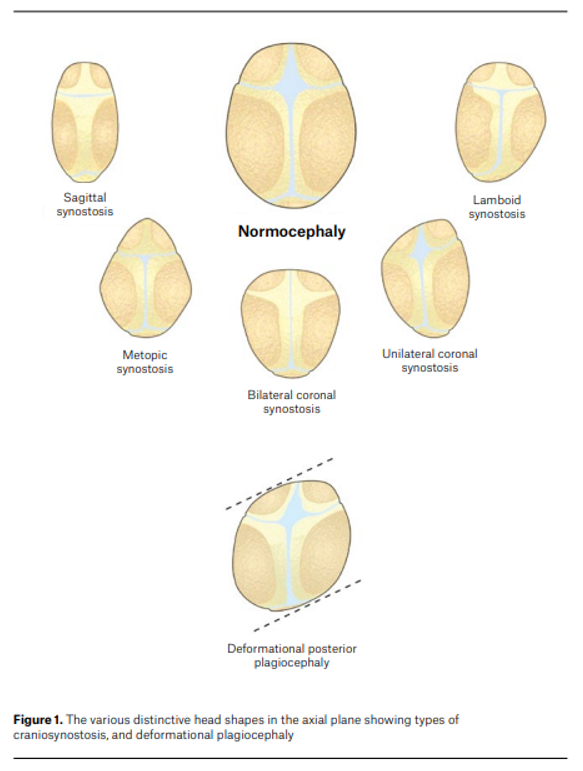
Craniosynostosis (or Synostotic Plagiocephaly)
- Rarer condition that may cause a variety of abnormal head shapes. It arises from premature fusion of one or more of the cranial sutures. Craniosynostosis tends to cause a progressive deformity with distinctive head shapes depending on the involved suture(s). It can be non-syndromic or associated with a syndrome (e.g. Apert, Crouzon). [Appendix 1 to view different types of head shapes]
Microcephaly
- Rare condition in which an infant’s head circumference (HC) is significantly smaller than expected relative to their age and growth parameters., It may be congenital or acquired and is often associated with underlying disturbances in brain development. Children with microcephaly may experience neurodevelopmental difficulties.
- Microcephaly is defined as:
- HC <3rd percentile for age
or
- Serial HC measurements that cross two or more centile lines downward
or
- HC that is disproportionately small relative to weight and length
Macrocephaly
- When the HC is > 98th percentile for age or disproportionately large when compared to other growth parameters. Benign / familial macrocephaly is the most common cause, however, there are other significant causes that should be considered.
Anterior fontanelle (AF)
- The AF size and time of closure is highly variable. The median time of closure is 14 months (range 3-24 months). This is affected by gender and ethnicity. In one study of Māori/Pacific Islander children the AF was closed in 25% at 4-61 months compared to 5% at 5 months in a North American group of infants2. ‘Early’ closure of the AF is not concerning but warrants further evaluation if there is also one or more of:
- Microcephaly: HC < 3rd percentile, disproportionately small compared to weight and length, or crossing more than 2 percentiles
- Significant developmental delay or syndromic features
- Ridging of sutures suggesting craniosynostosis
Pre-referral investigations
In general, there are
no investigations required for these referrals, noting:
- Do not perform skull x-rays – it will not change management.
- Positional plagiocephaly is a clinical diagnosis and no imaging is required.
Pre-referral management
- Positional Plagiocephaly:
- Reassure parents - most cases of positional plagiocephaly will resolve with conservative measures.
- Encourage parents to sleep baby on back as per SIDS guidelines
- Reposition baby’s head to their non-preferred side while sleeping
- Practice supervised tummy time and side lying every day while baby is awake
- Encourage baby to look in both directions by
- changing cot positions
- sleeping baby at opposite ends of the cot
- repositioning toys and mobiles
- alternating sides on which baby is held
- If torticollis is present, consider a referral to a Child Development Services physiotherapist or a private physiotherapist
- Monitor HC with serial measurements
- Helmet therapy is not used or recommended by Perth Children’s Hospital
- Macrocephaly:
- Parental and child HC can be plotted on the Weaver Curve. If the child’s HC falls within the range determined by the average parental score, a genetic contribution to macrocephaly is likely4.
When to refer
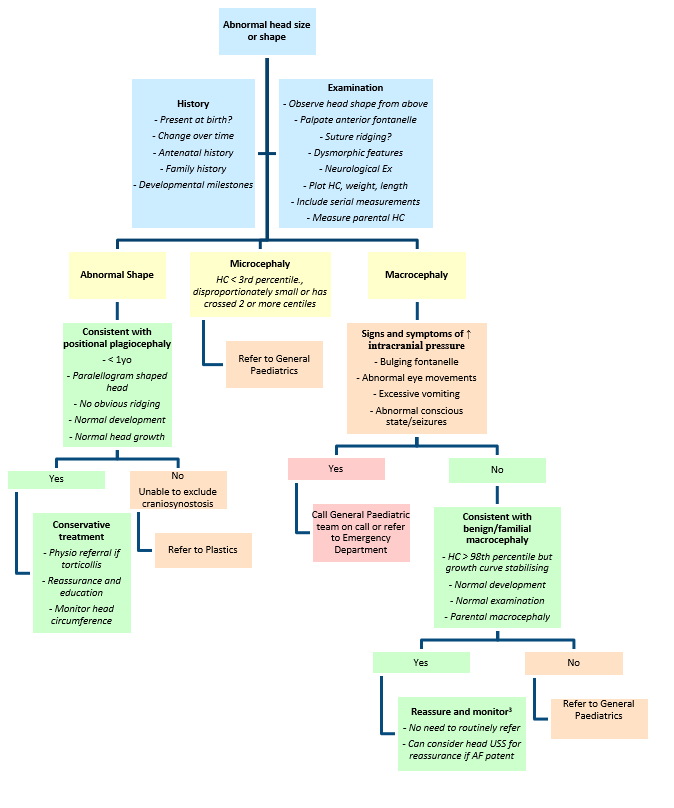
See flow chart above.
Refer to Perth Children’s Hospital
Plastics Department if:
- Concern of craniosynostosis
- Severe head shape anomaly
- Skull shape not typical of positional plagiocephaly
- Head shape worsening with time, not responding to conservative measures
- Ridging of sutures
Refer to General Paediatric Medicine if:
- Head circumference crossing more than 2 growth percentiles, disproportionate to weight and length and not consistent with benign familial macrocephaly
- Concerns regarding development
- Dysmorphic features
- Abnormal neurological examination
How to refer
- Routine non-urgent referrals from a GP or a Consultant are made via the Central Referral Service
- Routine non-urgent referrals from private hospitals are made via the PCH Referral Office (Fax: 6456 0097 or email PCH.Referrals@health.wa.gov.au)
- Urgent referrals (less than seven days) are made via the PCH Referral Office. Please call Perth Children’s Hospital Switch on 6456 2222 to discuss referral with the General Paediatrician on-call
Essential information to include in your referral
- History
- Perinatal history - positional plagiocephaly is associated with prematurity, restricted intrauterine environment, assisted delivery, prolonged labour, unusual birth position.
- Developmental history – please include Ages and Stages Questionnaire (ASQ)
- Growth parameters and percentile charts, especially head circumference
- For children born before 37 weeks gestation, please use Fenton’s growth chart.
- For macrocephaly, include parental head circumferences.
- Physical examination findings
- Skull shape, sutures and fontanelles
- Ear and eye position
- Eye movements
- Neck mobility or masses
- Spine, hip and general neurological examination
- Dysmorphic features
Appendix 1: Head shape5
References
- Kirkpatrick J, Bowie S, Mirjalili SA. Closure of the anterior and posterior fontanelle in the New Zealand population: A computed tomography study. J Paediatr Child Health. 2019;55(5):588-93.
- Pindrik J, Ye X, Ji BG, Pendleton C, Ahn ES. Anterior fontanelle closure and size in full-term children based on head computed tomography. Clin Pediatr (Phila). 2014;53(12):1149-57.
- Suspected neurological conditions: recognition and referral. National Institute for Health and Care Excellence (NICE): Guidelines. London 2019.
- Weaver DD, Christian JC. Familial variation of head size and adjustment for parental head circumference. J Pediatr. 1980;96(6):990-4.
- Lun KK, Aggarwala S, Gardner D, Hunt J, Jacobson E, Reddy R, et al. Assessment of paediatric head shape and management of craniosynostosis. Aust J Gen Pract. 2022;51(1-2):51-8.
- Thomas CN, Kolbe AB, Binkovitz LA, McDonald JS, Thomas KB. Asymptomatic macrocephaly: to scan or not to scan. Pediatr Radiol. 2021;51(5):811-21.
- Kiesler J, Ricer R. The abnormal fontanel. Am Fam Physician. 2003;67(12):2547-52.
- Hersh DS, Bookland MJ, Hughes CD. Diagnosis and Management of Suture-Related Concerns of the Infant Skull. Pediatr Clin North Am. 2021;68(4):727-42.
- Furtado LMF, Filho J, Freitas LS, Dantas Dos Santos AK. Anterior fontanelle closure and diagnosis of non-syndromic craniosynostosis: a comparative study using computed tomography. J Pediatr (Rio J). 2022;98(4):413-8.
- Accogli A, Geraldo AF, Piccolo G, Riva A, Scala M, Balagura G, et al. Diagnostic Approach to Macrocephaly in Children. Front Pediatr. 2021;9:794069.
| Approved by: |
General Paediatrics Department |
Date: |
July 2025 |
| Endorsed by: |
General Paediatrics Department |
Date: |
July 2025
|
This document can be made available in alternative formats on request for people with disability.